United Healthcare Insurance
Navigating the world of health insurance doesn’t have to be overwhelming. If you have United Healthcare insurance or are curious about United Healthcare plans, you may be wondering whether UnitedHealthcare insurance covers substance use treatment.
Deciding to enter a substance use treatment program can be one of the most important decisions of your life. It is important to understand your insurance coverage and the treatment options available to you based on your specific insurance plan. Rehabilitation centers can check and verify your coverage based on the information you provide.
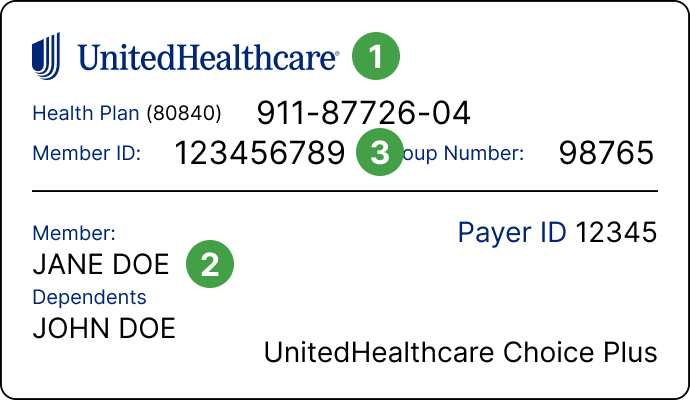
UnitedHealth Group (also known as UHC) is comprised of 2 companies–United Healthcare and Optum–and offers healthcare plans in all 50 states and 130 countries.6 United Healthcare provides healthcare insurance for over 28 million Americans. The specifics of your coverage depend on your state and your plan. To understand what services are covered under your United Healthcare insurance plan, call the number on the back of your insurance card.
Coverage Levels
United Healthcare’s Medicare Advantage Plan covers services such as medical detoxification in a substance use treatment facility—or in a hospital setting if medically necessary—as well as inpatient and outpatient rehabilitation (including individual and group therapy).2 There are no limits to the number of outpatient program sessions you receive; extended stay in a drug and alcohol rehabilitation program is also covered if medically necessary.2
UHC Choice and Choice Plus plans allow you to select your in-network provider without a referral. However, there may be additional costs if you receive services that are outside of United Healthcare’s network. Most preventative care services are completely covered under this plan.
Choice Advanced and Choice Plus Advanced have lower co-pays and greater co-insurance. You are still required to receive services with an in-network provider, although you don’t have to select a primary care physician with this plan. UHC also offers preferred-provider organization plans that may require referrals for services; some allow out-of-network services, although your out-of-pocket costs will be higher if you choose an out-of-network provider.
Does United Healthcare Cover Drug or Alcohol Rehab?
Like many insurance providers, United Healthcare insurance covers some, if not most, of the costs associated with mental health and substance use treatment. United Healthcare (UHC) insurance offers a number of plans for individuals, families, and employers as well as Medicaid and Medicare plans.1 Coverage is determined by factors including your budget, health status, current and future health needs, and location. If you have United Healthcare and are looking for substance use treatment services, many of your treatment services may be covered.
There is no one-size-fits-all solution when it comes to substance use disorder treatment. People struggling with addiction have different needs. Therefore, an individualized treatment plan begins with an assessment from a licensed clinician, who evaluates your substance use, physical and mental health needs, your social supports, and more to determine the right level of care for you.
Substance use disorder treatment may involve a combination of services and can include:
- Detoxification (for some substances).
- Individual counseling.
- Group therapy.
- Behavioral therapies.
- Medication for addiction treatment.
- Psychoeducation.
- Community recovery services, such as mutual-help groups.
These services may take place in an outpatient, inpatient, or combination of outpatient and inpatient settings, depending on your individual plan and how you progress through treatment.
Outpatient Treatment
Outpatient care, which allows you to live at home or in a sober living environment while participating in a treatment program, my be a point of entry in the continuum of care for some individuals. And for others, it may be a step down from a more intense level of treatment. Regardless, outpatient care generally involves many of the services listed above and may be covered by your United Healthcare insurance plan, depending on your needs and policy. Covered services may include outpatient therapy, intensive outpatient programs (IOPs), and/or partial hospitalization programs (PHPs). Each level of outpatient care varies in intensity, duration, and cost. Therefore, it is important to check with your insurance provider to determine what’s covered by your specific plan.
Inpatient Treatment
Depending on your needs and policy, your United Healthcare insurance plan may cover all or a portion of local, short-term, intensive residential treatment, which includes the services listed above as well as room and board for the duration of treatment. Call United Healthcare to understand your coverage for inpatient care, including the length of stay.
How To Pay for Rehab with United Healthcare Insurance
American Addiction Centers (AAC) is a leader in providing effective substance use treatment in facilities across the country. AAC can verify that your United Healthcare plan is accepted at your chosen facility, since most AAC facilities are in-network drug treatment providers with United Healthcare. You can verify your insurance coverage to immediately see whether the facility is an in-network provider. Or call to speak with a knowledgeable admissions navigator.
AAC’s compassionate admissions navigators are available 24/7 to help answer questions you may have about your addiction or your loved one’s addiction. The call is 100% confidential. AAC understands how difficult it can be to make the decision to end an addiction and get treatment. AAC’s admissions navigators can help you understand your options and help you find your path to recovery.
Does United Healthcare Insurance Cover Mental Health Care & Co-Occurring Disorders?
Under the Affordable Care Act (ACA), most insurance companies that offer individual and small company coverage are required to cover mental health and substance use services.2 United Healthcare’s mental health and substance use treatment coverage is available in many of their plans.
Functionality and quality of life are significantly impacted by mental health and substance use problems. The ACA ensures coverage for people who struggle with co-occurring disorders—that is, both mental health and substance use disorders. Treating these issues is as important as treating physical health problems. In fact, in order for substance use treatment to be effective, mental health and addiction treatment must be addressed simultaneously.
Failure to treat a mental health disorder can significantly impact your recovery. Neglecting the underlying contributors to addiction, such as mental health illnesses, may make you more vulnerable to relapse in the future.
How Long Does United Healthcare Insurance Cover Rehab?
Many factors go into determining the type of substance use treatment interventions and rehab services you will receive, and for how long. Where you live, the available treatment facilities, your age, underlying mental and physical health concerns, length of substance use, severity of the substance use disorder, the types of substances used, and your insurance coverage factor in to the creation of your personalized treatment plan. This, along with your progression through treatment determine the amount of time you spend in treatment, which is different for every person.
The facility you choose can work with you and United Healthcare to determine the most appropriate duration of treatment for you. Research shows, however, that people who remain in substance use treatment for longer amounts of time are more likely to achieve their recovery goals.4
What if My United Healthcare Insurance Policy Does Not Cover Drug Addiction Treatment?
If your insurance plan doesn’t cover drug treatment services, there are other ways to pay for treatment. Other options include:
- Private pay. Simply put, private pay means you find a way to fund your treatment on your own. This may involve using savings or credit or borrowing from family or friends.
- Grants or scholarships. Some treatment centers offer grants and scholarships to help those in need pay for their treatment. You can talk directly to the treatment facility or look into nonprofit organizations in your area. The Substance Abuse and Mental Health Services Administration (SAMHSA) offers grants, too.
- Financing and sliding fee scales. Some rehab facilities offer financing or payment plans that allow you to spread the cost of addiction treatment out as opposed to paying it all at once up front. Additionally, some treatment centers provide sliding fee scales, meaning your cost is based on your income.
- Crowdfunding or fundraising. You may use a crowdfunding site to ask family, friends, even strangers to donate money to help you cover the cost of treatment.
Cost should never be a barrier to treatment. When you seek treatment, you are making an investment in your health, well-being, and future.
Do Treatment Centers Need To Be In Network?
No, treatment centers do not need to be an in-network provider for United Healthcare insurance to cover at least part of substance use treatment. However, this is all dependent on your plan.
By definition, in-network providers are providers, suppliers, and facilities that have contracts with your insurance provider.5 Out-of-network providers are providers, services, and facilities that do not have a contract with your particular insurance provider.
Your plan may be a health maintenance organization (HMO) or a preferred provider organization (PPO). The main differences involve out-of-pocket and monthly costs and your ability to choose providers. With an HMO, you pay lower monthly premiums and are required to choose in-network providers. Failing to do so could mean that your services aren’t covered. PPOs usually have higher monthly premiums and out-of-pocket costs, but you choose your in- or out-of-network providers.
You can contact United Healthcare to verify your substance use coverage and confirm whether the treatment facility you choose is an in-network provider. You can also contact the treatment facility to confirm that they accept your insurance and your specific plan.
What Rehab Centers Accept United Healthcare Insurance?
American Addiction Centers (AAC) has various inpatient and outpatient rehab centers located around the country that provide drug and alcohol addiction treatment. If you have a United Healthcare insurance plan, the following AAC facilities accept United Healthcare insurance for drug and alcohol addiction rehab:
- AdCare Rhode Island: With multiple facilities located in Rhode Island, AdCare provides innovative, quality, and cost-efficient addiction treatment. Its integrated system of care offers an inpatient treatment center in North Kingstown and an outpatient facility in Warwick. AdCare’s continuum of care includes detox services, residential treatment, co-occurring disorder treatment, intensive outpatient services, outpatient services, and tele-health.
- AdCare Hospital and Outpatient Center: Located in Worcester, Massachusetts, AdCare offers safe medical detox, intensive outpatient services, and partial hospitalization services.
- Recovery First Treatment Center: Located in Hollywood, Florida, Recovery First treats substance use disorders by combining evidence-based therapeutic modalities with top-level care. Recovery First provides a complete continuum of care including detox services, residential care, co-occurring disorder treatment, intensive outpatient services, outpatient services, and tele-health.
- River Oaks Treatment Center: Located in Riverview, Florida, River Oaks provides top-level care for addiction and mental health disorders. River Oaks provides a complete personalized continuum of care, which includes detox, residential treatment, co-occurring disorder treatment, intensive outpatient services, and a partial hospitalization program. Later this year, River Oaks will also offer primary mental health treatment for individuals suffering from a mental illness without a substance use disorder.
- Oxford Treatment Center: Oxford offers evidence-based therapies and an opportunity to connect with nature and try new activities. Provided care includes detox, residential treatment, and co-occurring disorder treatment at the treatment center in Etta, Mississippi. In nearby Oxford, at the outpatient treatment center, intensive outpatient and partial hospitalization programs are offered. And in Southaven, AAC’s newest treatment facility now provides outpatient services to the Memphis metropolitan area.
- Laguna Treatment Center: AAC’s Southern California treatment center, located in Aliso Viejo, provides safe medical detox, inpatient residential care, and co-occurring disorder treatment. Laguna Treatment Center is an in-network provider with United Healthcare for some services. Check with Laguna or your insurance provider to confirm that the treatment you need is a covered service.
- Desert Hope Treatment Center: Located in Las Vegas, Nevada, Desert Hope provides the full continuum of care, including detox services, residential treatment, co-occurring disorder treatment, and intensive outpatient services. Desert Hope Treatment Center is an in-network provider with United Healthcare for outpatient services only.
In-network rehab facilities are approved or have a contract with United Healthcare insurance to offer services at a set price. This means that your out-of-pocket expenses will typically be lower than if you choose an out-of-network rehab center. In some cases, you may even be responsible for the full cost of substance use rehab if you choose an out-of-network facility.
Call AAC at to speak to an admissions navigator, who can help you begin your recovery journey today.
Sources
- UnitedHealthcare. (n.d.). Health insurance plans.
- U.S. Department of Health and Human Services. (2019). Does the Affordable Care Act cover individuals with mental health problems?
- UnitedHealthcare. (2020). Coverage summary.
- U.S. National Library of Medicine. (n.d.). Chapter 5- Specialized substance abuse treatment programs.
- U.S. Centers for Medicaid & Medicaid Services. (n.d.). Network.
- UnitedHealth Group. Who We Are.