Aetna Insurance Coverage for Alcohol and Drug Rehab Treatment
The Affordable Care Act (ACA) requires that most insurance plans (small employer, individual, ACA Marketplace) provide basic coverage for behavioral health services.1 Behavioral health services include both mental health and treatment for substance use disorder (SUD).1
This applies to most Aetna plans; however, the extent of this coverage will vary depending on the individual insurance policy.
Aetna Insurance Coverage for Alcohol and Drug Rehab Treatment
Founded in 1853 and active in all 50 states, Aetna’s network coverage includes 1.2 million healthcare professionals, almost 700,000 primary care doctors and specialists and over 5,700 hospitals.2 The company has over 46 million members in its various health plans, including regular health insurance, dental insurance, and vision insurance.3
Aetna insurance plans should provide coverage for drug and alcohol rehab, and Aetna coverage is accepted at many American Addiction Centers (AAC) facilities.
Types of Aetna Insurance Plans
The amount your Aetna insurance will cover will depend on the specific Aetna plan you have.1
Aetna offers a variety of plans:4
- Health maintenance organization (HMO) plans have low monthly premiums and deductibles and often require that you pay a copayment when you visit doctors, specialists, and hospitals.
- Point of service (POS) plans require that you select a primary care provider (PCP) who will provide you with referrals to see specialists as needed.
- Exclusive provider organization (EPO) plans cover only in-network services but generally have a much more extensive network than other plans.
- Preferred provider organization plans do not require PCP referrals for in-network or out-of-network services. PPO plans typically have low copayments but high monthly premiums.
- High deductible health plans have higher deductibles and lower monthly premiums than some plans and often offer a healthcare savings account to help offset out-of-pocket expenses.
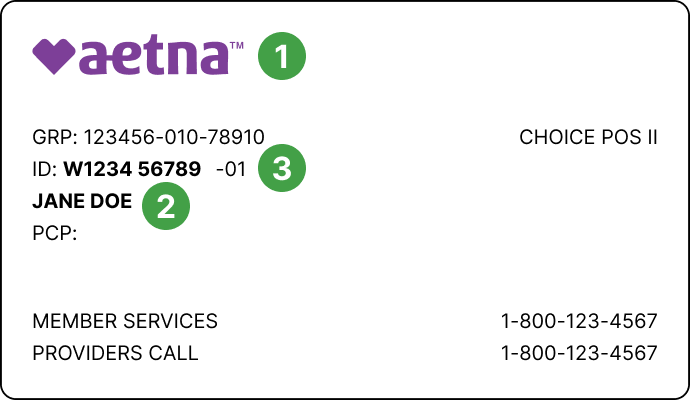
To learn more about your Aetna drug rehab coverage, you can call the number on the back of your Aetna insurance card. Many drug rehab centers are also able to verify your Aetna coverage.
Aetna Rehab Coverage
Aetna will cover all or some of your drug rehab treatment, depending on your specific plan and the types of services you seek. Drug rehab services may include the following levels of care:5, 6,7,8
- Medical detox, which is often the first step in addiction treatment. Detox can be provided in inpatient or outpatient settings, depending on the facility. During medically assisted detox, treatment staff will supervise you or your loved one through acute withdrawal, ensuring they remain safe and stable before transitioning to another level of addiction treatment. While crucial for many,
- Inpatient/residential rehab, which requires you or your loved one to live at a drug rehab center temporarily. During inpatient/residential rehab, you may receive medical detoxification; medication-assisted treatment program; individual, group, or family therapy; drug education; relapse prevention; or life skills classes. You may also be required to participate in 12-step programs.
- Outpatient rehab, which allows you or your loved one to remain in the comfort of your home while receiving drug rehab services at a community center, doctor’s office, rehab facility, or other location. Many of the same treatment methods used in inpatient rehab are employed in outpatient treatment. There are varying levels of outpatient care. From most intensive to least intensive, these range from partial hospitalization programs (PHPs), to intensive outpatient programs (IOPs), to standard outpatient care
Does Aetna Insurance Cover Mental Health Care Treatment Facilities?
Yes, mental health care is covered by Aetna.
Under the ACA, all insurance plans must provide at least basic behavioral health treatment coverage, which includes both mental health and substance abuse care.1 Sometimes, people suffer from mental health and substance abuse issues that occur simultaneously. Co-occurring disorders are pretty common. Study results have shown that roughly 53 percent of people with a substance use disorder are also diagnosed with a mental health disorder.9
Your Aetna insurance plan will determine how much coverage you’ll have for the specific mental health care services you receive.
How Long Does Aetna Insurance Cover Rehab?
The length of time Aetna will cover rehab services depends on the specific plan and the types of services involved. There are many coverage levels within the Aetna insurance plans. Each level is associated with different monthly premiums, deductibles, and coverages.1,4 There are also many different types and levels of drug rehab services.
Aetna drug rehab services are tailored to meet each person’s specific needs. Research indicates that more extended treatment is most effective. People engaging in long-term treatment (90 days or longer) are more likely to remain abstinent 6 months later. They are also less likely to experience homelessness.10,11
If you have Aetna, verify benefits for Aetna drug coverage by calling the number on the back of your Aetna insurance card or visiting the Aetna insurance website. Many drug rehab centers are also able to verify your Aetna insurance plan coverage.
What If My Aetna Insurance Policy Does Not Cover Rehab?
If your Aetna insurance plan does not cover drug rehab services, some facilities offer:
- Payment plans.
- Sliding scale fees (i.e., charging less for patients with lower incomes).
- Scholarships.
There are also some nonprofit organizations that provide funding for drug rehab services.
Aetna In-Network vs. Out-of-Network Rehab Centers
The Aetna rehab provider network consists of an extensive network of Aetna-approved providers, such as doctors, specialists, hospitals, and facilities. To be in-network means that a doctor, specialist, hospital, or facility has a contract to provide services to Aetna policyholders, often for a cheaper rate. Providers and facilities that do not contract Aetna are considered out-of-network, and you’re likely to be charged a much higher rate for their services. If the provider is out-of-network, the policyholder would be responsible for covering the extra cost of care.13
To verify a provider’s network status, you can visit the Aetna website or call the number on the back of your Aetna insurance card.
What Rehab Centers Take Aetna Insurance?
American Addiction Centers (AAC) has various rehab facilities around the country that provide drug and alcohol addiction treatment. If you have a Blue Cross Blue Shield insurance plan, the following AAC facilities accept Blue Cross Blue Shield for drug and alcohol addiction rehab.
- AdCare Rhode Island: With various facilities located in Rhode Island, AdCare provides innovative, quality, and cost-efficient addiction treatment. Its integrated system of care offers an inpatient treatment center in North Kingstown and a network of outpatient offices throughout Rhode Island. AdCare’s continuum of care includes detox services, residential treatment dual-diagnosis treatment, intensive outpatient services, inpatient and outpatient services, and tele-health.
- Greenhouse Treatment Center: Located in Grand Prairie, Texas, Greenhouse offers individualized treatment plans and many levels of care including detox services, residential treatment, dual-diagnosis treatment, intensive outpatient services, outpatient services, and tele-health, all in a luxurious setting with high-end amenities.
- Oxford Treatment Center: Located in Etta, Mississippi, Oxford offers gender-specific rehab while offering an opportunity to connect with nature and try new activities. Provided care includes detox, residential treatment, dual-diagnosis treatment, inpatient and outpatient treatment, intensive outpatient services, and tele-health, all with individualized treatment programs.
- Recovery First Treatment Center: Located in Hollywood, Florida, Recovery First treats substance use disorders by combining evidence-based therapeutic modalities with top-level care. Recovery First provides a personalized continuum of care including detox services, residential treatment dual-diagnosis treatment, intensive outpatient services, outpatient services, and tele-health.
- River Oaks Treatment Center: Located in Riverview, Florida, River Oaks treats substance use disorders through combining evidence-based therapies with world-class amenities. Provided care includes detox, residential treatment, behavioral disorder treatment, dual-diagnosis treatment, outpatient services, and tele-health, all with individualized treatment programs.
There are various treatment programs for individuals struggling with drug or alcohol addiction, so don’t give up if the first program you check out doesn’t meet your individual needs. There are rehabs near you that can provide the treatment you need. Check out the directory to find a list of facilities and programs. You can search by location and filter by Aetna insurance.
How to Check Aetna Rehab Coverage?
Some drug rehab centers can provide instant verification of your Aetna insurance benefits. American Addiction Centers provides a 24/7 helpline to connect you with knowledgeable and understanding admissions navigators who can verify insurance coverage for you or your loved one. Simply call to speak to an admissions navigator.
You can also check your insurance benefits by calling the number on the back of your Aetna insurance card or visiting the Aetna insurance website.
Sources
- American Addiction Centers. (2020). Aetna covered drug and alcohol treatment rehabs.
- (2021). HMO, POS, PPO, EPO, and HDHP with HSA: What’s the difference?
- American Addiction Center. (2021). How to choose an inpatient drug rehab.
- American Addiction Centers. (2020). Frequently asked questions about outpatient treatment.
- American Addiction Centers. (2021). What is an intensive outpatient program?
- American Addiction Centers. (2020). Drug rehab guides for addiction & mental health.
- Missouri Department of Mental Health. (2021). Co-occurring psychiatric and substance use disorders.
- Drake, R., Mueser, K., & Brunette, M. (2007). Management of persons with co-occurring severe mental illness and substance use disorder: Program implications. World Psychiatry, 6(3), 131 – 136.
- American Addiction Centers. (2021). Co-occurring disorder and dual diagnosis treatment guide.
- Brunette, M., Drake, R., Woods, M., & Hartnett, T. (2001). A Comparison of long-term and short-term residential treatment programs for dual diagnosis patients. Psychiatric Services, 52(4), 526 – 528.
- Proctor, S., & Herschman, P. (2014). The continuing care model of substance use treatment: What works, and when is “enough,” ‘‘enough?’’ Psychiatry Journal, 14(3), 1 – 16.
- Ornell, F., Moura, H., Scherer, J., Pechansky, F., Kessler, F., & Diemen, L. (2020). The COVID-19 pandemic and its impact on substance use: Implications for prevention and treatment. Psychiatry Research, 289, 1 – 2.
- (2021). Aetna insurance coverage for drug and alcohol rehab treatment.
- (2021). Network and out-of-network care.
- (2021). Provider referral directory.
- Aetna. (n.d.). Aetna Home Page.
- Aetna. (n.d.). Aetna Facts.