Does BlueCross BlueShield Cover Addiction Treatment?
Yes. BlueCross BlueShield (BCBS) covers addiction treatment.1 As one of the nation’s largest and oldest insurance providers, BCBS is generally accepted at many drug and alcohol rehabs, including American Addiction Centers. However, specific coverage details can vary based on your state of residence, your individual plan, and the specifics of your policy. Depending on your plan, BCBS may cover various addiction treatment services like inpatient rehab, outpatient programs, medication-assisted treatment, and therapy.
Rehabs That Take Blue Cross Blue Shield Insurance
American Addiction Centers (AAC) has various rehab facilities around the country that provide drug and alcohol addiction treatment. If you have a Blue Cross Blue Shield insurance plan, the following AAC facilities accept Blue Cross Blue Shield for drug and alcohol addiction rehab.
- AdCare Treatment Centers: With multiple locations throughout Massachusetts and Rhode Island, AdCare has been a trusted provider of addiction treatment. Their team of experienced professionals is dedicated to delivering personalized care, whether you require inpatient or outpatient services.
- Desert Hope Treatment Center: Located in Las Vegas, offers a full range of personalized addiction treatment programs, including detox, residential, dual-diagnosis, intensive outpatient, and telehealth services.
- Greenhouse Treatment Center: Located in Grand Prairie, Texas, Greenhouse offers individualized treatment plans and many levels of care including detox services, residential treatment, dual-diagnosis treatment, intensive outpatient services, outpatient services, and tele-health, all in a luxurious setting with high-end amenities.
- Laguna Treatment Center: Located in Orange County, California, Laguna is a chemical dependency recovery hospital that focuses on treating people who are medically compromised and need 24/7 oversight. Provided care includes detox services, residential treatment, dual-diagnosis treatment inpatient treatment, and intensive outpatient services.
- Oxford Treatment Center: Located in Etta, Mississippi, Oxford offers gender-specific rehab while offering an opportunity to connect with nature and try new activities. Provided care includes detox, residential treatment, dual-diagnosis treatment, inpatient and outpatient treatment, intensive outpatient services, and tele-health, all with individualized treatment programs.
- River Oaks Treatment Center. Located in the Tampa, FL metro area, prioritizes individualized care for every patient on their journey to recovery. As an American Addiction Centers (AAC) facility, they leverage the expertise of industry leaders to provide the highest quality treatment. The team at River Oaks is committed to utilizing the latest research and best practices to ensure each patient receives the most effective and compassionate care possible.
- Recovery First Treatment Center. Located in Hollywood, Florida, Recovery First offers comprehensive addiction rehab services to the greater Miami area. Specializing in inpatient alcohol and drug rehab, they also provide outpatient programs and a continuum of care for adults struggling with addiction and co-occurring mental health disorders.
There are various treatment programs for individuals struggling with drug or alcohol addiction, so don’t give up if the first program you check out doesn’t meet your individual needs. There are rehabs near me that can provide the treatment you need. Check out the directory to find a list of facilities and programs. You can search by location and filter by Blue Cross Blue Shield insurance.
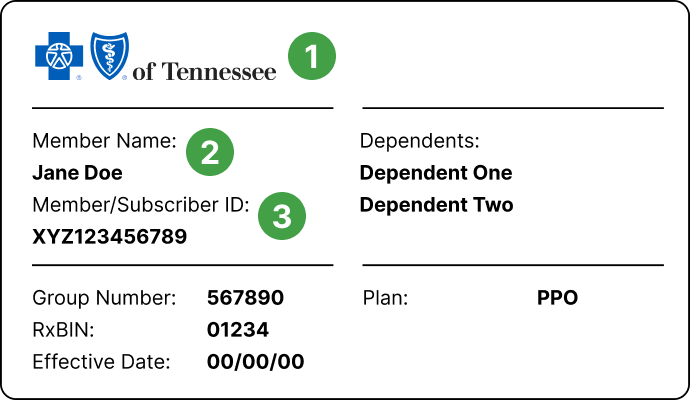
How to Check Your BlueCross BlueShield Rehab Coverage
There are many different ways to check your BCBS benefits.
- Visit your local BCBS company website and verify your benefits through their online portal.
- Speak with your plan administrator through your employer.
- AAC offers several ways to find out what type of addiction treatment coverage you have through BCBS.
- Call us at and speak with an admissions navigator.
- Fill our our safe, secure, and confidential insurance verification form.
What Will Blue Cross Blue Shield Insurance Cover?
Depending on your specific plan, BCBS Insurance may cover a portion or the entire cost of drug rehab. The levels of rehab care include:6
- Inpatient/residential rehab—You or a loved one live at the facility throughout the duration of treatment, which is typically anywhere from a few weeks to several months in length. You will receive 24-7 care from medical professionals, as well as attend individual and group counseling.
- Intensive outpatient program (IOP)—An IOP is a type of outpatient treatment program that is more structured than a standard outpatient program, but less intensive than an inpatient facility. While it doesn’t require living at the treatment facility, it does require more frequent visits (at least 9 hours a week). IOPs also involve care from medical professionals including doctors, nurses, therapists, psychologists, and social workers.
- Partial hospitalization programs (PHP)—PHP services are another type of outpatient treatment for people who require more supervision than a traditional outpatient program offers, but not as much supervision as an inpatient program. This type of program usually takes place in a hospital setting and requires approximately 20 hours of treatment per week. It involves both individual and group counseling, and may also provide medication-assisted treatment to address withdrawal symptoms.
- Outpatient rehab—Outpatient rehab services allow patients to continue living at home while they attend sessions a few times per week.
Does Blue Cross Blue Shield Insurance Cover Mental Health Care?
The Affordable Care Act requires that all insurance plans provide coverage for behavioral health services, including mental health and substance abuse issues.1 Many BCBS insurance plans cover individual therapy and other services for people with co-occurring disorders. Coverage levels will vary, so it’s important to check your benefits. Additionally, you or a loved one may have to pay some costs such as a copayment or the remaining balance of the plan’s deductible.
How Long Will BlueCross BlueShield Insurance Cover Rehab?
There is no specified period that BCBS insurance or any insurance will cover drug rehab services. This is because many factors determine coverage, such as the specific plan’s parameters, the location of the drug rehab program, and the person’s treatment needs. However, some study results have shown that people who remain in treatment for 3 months or longer are more likely to have positive treatment outcomes (i.e., abstinence from drugs and/or alcohol).7
What if My BlueCross BlueShield Insurance Does Not Cover Rehab?
Even if your BCBS insurance doesn’t fully cover rehab, there are still ways to access treatment. Many facilities offer flexible payment plans or scholarships to help make it affordable. You can also explore nonprofit organizations and grants that provide financial assistance for addiction treatment.
Money should not keep you or a loved one from getting the treatment you need so you can live the life you deserve. Give us a call at to discuss your payment options.
How Do I Pay for Costs Not Covered by BlueCross BlueShield Insurance?
If your BCBS insurance doesn’t cover all rehab costs, you have options:
- Flexible Payment Plans: Many facilities offer manageable payment plans to spread out costs.
- Scholarships & Grants: Some centers and nonprofits provide financial aid for treatment.
- HSA/FSA: If you have a Health Savings Account or Flexible Spending Account, you can use these pre-tax dollars to cover eligible out-of-pocket expenses.
Blue Cross Blue Shield Insurance Plan Options
BCBS Insurance plans are provided at different levels, each with its own monthly premiums and deductibles.3 A deductible refers to the amount of money you will pay before your insurance is activated. The following is a breakdown of the different insurance plan levels offered by BCBS:3
- Bronze: These plans typically cover about 60% with high deductibles and low monthly premiums.
- Silver: These plans typically cover about 70%. Deductibles are low, but monthly premiums are higher than bronze plans.
- Gold: These plans typically cover about 80% with lower deductibles and higher monthly premiums than the bronze and silver plans.
- Platinum: Platinum plans are not available in all states or locations. These plans typically cover about 90% and have low deductibles and very high monthly premiums compared to the bronze, silver, and gold plans.
In addition to the level of plan chosen, your monthly premium and plan deductible under BCBS Insurance is also determined by whether you choose a Health Maintenance Organization (HMO) plan or a Preferred Provider Organization (PPO) plan.4
BCBS offers both HMO and PPO plans.
- An HMO plan allows you to select a primary care physician (PCP) who will provide you referrals for other providers, hospitals, and specialty clinics within your network as needed.4 HMO plans typically have lower monthly premiums but higher deductibles.4
- With a PPO plan, you will not need to choose a PCP, and you are not confined to a network.4 You can visit any provider, hospital, or specialty clinic. PPO plans often have higher monthly premiums but lower deductibles.4
- BCBS also offers a Health Savings Account (HSA), which allows you to save money for your healthcare-related expenses.3
BCBS insurance is connected to a large network of providers. These providers are referred to as in-network. Providers outside of this network are out-of-network.
If you or a loved one has a BCBS HMO plan, you may be required to obtain a referral from your PCP to receive drug rehab services, and you must use drug rehabs that are only in-network.4 With a BCBS PPO plan, you may not need a referral, and you may use any in-network or out-of-network facility.5
About BlueCross BlueShield
BCBS insurance consists of 35 independent and locally operated companies across all 50 states, the District of Columbia, and Puerto Rico.2 In the U.S., 1 in 3 Americans are covered by an individual or family BCBS insurance plan.2 BCBS also offers employer-sponsored insurance plans and insurance plans specifically designed for federal employees.1 Over 5 million federal employees, retired federal employees, and their families are covered under the federal BCBS plan.2 BCBS also provides international insurance plans for people who live, work, or travel outside of the U.S.2
Frequently Asked Questions
Sources
- American Addiction Centers Treatment Solutions. (2021). Does Blue Cross Cover Drug and Alcohol Rehab Insurance?
- Blue Cross Blue Shield. (2021). BCBS Companies and Licensees.
- Blue Cross Blue Shield. (2021). What’s the difference between bronze, silver, and gold plans?
- Blue Cross Blue Shield Blue Care Network of Michigan. (2021). What’s the difference between HMO and PPO plans?
- Blue Cross Blue Shield: Substance Use Resource Center. Supporting Your Journey to Recovery.
- John Hopkins Medicine. Center for Substance Abuse Treatment and Research. Treatment Settings.
- National Institute on Drug Abuse. (2018). Principles of Drug Addiction Treatment: A Research-Based Guide (Third Edition).
- Blue Cross Blue Shield of Texas. Types of Health Insurance Coverage.
- Blue Cross Blue Shield. Substance Use Resource Center.
- Blue Cross Blue Shield. (2021). Centers for Substance Use Treatment and Recovery: Directory of Providers.
- Centers for Medicare and Medicaid Services. The Mental Health Parity and Addiction Equity Act (MHPAEA).
- Blue Cross Blue Shield. (2017). Medicaid: A Primer on America’s Biggest Health Insurance Program.
- Department of Health and Human Services. (2020). Mandatory Medicaid State Plan Coverage of Medication Assisted Treatment.
- Department of Health and Human Services. (2019). Implementation of Section 5052 of the SUPPORT for Patients and Communities Act – State Plan Option under Section 1915(l) of the Social Security Act.