Veteran Drug & Alcohol Rehab Near Me
Veterans who are returning home from combat face a myriad of challenges during their transition back to civilian life. In 2018, according to U.S. Department of Veterans Affairs research, 1.7 million veterans received mental health treatment through the VA’s mental health specialty program.1, para 1 There are many issues those returning from combat may face, including, but not limited to, post-traumatic stress disorder (PTSD), substance use disorder, and other trauma or mental illness.2, para 1
Specifically, the National Institute of Drug Abuse cites that between 37% and 50% of returning Afghanistan and Iraq vets were diagnosed with a mental disorder that is associated with substance use disorder (SUD).3 What’s more, 63% of those diagnosed with SUD also met the criteria for having PTSD.3
As you can see, addiction, SUD, and co-occurring disorders are common occurrences among returning veterans. If you or a loved one is struggling with mental health or SUD following a return to civilian life, know that you’re not alone. There’s no shame in reaching out to get the care and support that you need.
Addiction and Substance Abuse Among Veterans
The stresses of deployment and active duty are often heavily associated with drug use, smoking, and unhealthy drinking.3, para 1 While the military’s zero-tolerance policies and random drug testing exist to help prevent addiction and substance use, they can also reinforce the stigma that prevents those in need of treatment from getting the care that they need.3, para 1
While in active duty, if you’re found to be using illicit drugs, you could be prosecuted or dishonorably discharged.3, para 2 However, when a veteran returns home, substance use and mental health issues become more common and concerning.3, para 2 Specifically among veterans, chronic pain, suicide risk, trauma, and homelessness contribute to substance use.3, para 3 As such, it’s estimated that more than 1 in 10 veterans are diagnosed with an SUD.3, para 3
Veteran Alcohol Abuse
Alcohol use disorder (AUD) and SUD are extremely common in both active-duty service members and veterans. Because active-duty service members are subject to random drug testing and face harsh penalties should they fail a drug test, many turn to alcohol when serving on tour. 3, para 1 For many on tour, they are exposed to a drinking culture, and these habits could potentially continue on following their return home.
What’s more, if service members were exposed to combat, violence, and trauma, they are at an increased risk of problematic drinking.3, “Alcohol – Active Duty” AUD isn’t limited to active-duty service members; veterans are at risk too. In 2020, it was found that nearly 1 million veterans had AUD and 4 million had a mental illness and/or SUD.4
Veteran Drug Abuse
Nearly 1 in 3 veterans who return to civilian life live with some form of chronic pain.5 This pain can lead to poor quality of life and can leave them at risk for developing an opioid dependence or addiction if opioid painkillers are prescribed for treating pain or injury.5 Although the VA’s Opioid Safety Initiative has helped reform the number of veterans being prescribed opioids and lower the dosage of prescriptions for those with an active prescription, addiction still persists.5
Beyond opioid use and addiction, veterans may also turn to other drugs to cope with the challenges they may be facing. PTSD is prevalent in the veteran population and can be extremely challenging to overcome, with many using substances to cope with their PTSD. More than 2 in 10 veterans with PTSD have SUD, and 1 in 3 seeking treatment for SUD also has PTSD.6 Many rehab services, particularly those offered by the VA, have programs dedicated to helping those with PTSD recover and lead a normal, fulfilling life.
Reasons for Veterans Substance Abuse
There are a wide variety of factors that may contribute to a veteran’s substance use. Environmental factors, demographics, and the onset of other mental health conditions can all contribute to a veteran turning to substances to cope.2 para 1Some of the most common potential contributing factors to alcohol and drug abuse include:
- PTSD: For many veterans, PTSD is common. It can occur in anyone but is common with service members, as it occurs after someone has experienced something traumatic, which could include combat, assault, natural disaster, or serious accident. PTSD is typically characterized as having flashbacks of the event, being on edge, heightened reactions, anxiety, night terrors, and depression.7 Nearly 1 in 3 veterans in treatment for PTSD have SUD.7
- Depression: Depression affects millions of Americans every year, including veterans. About 11% of the veteran population self-reported depressive symptoms or disorder.8
- Anxiety: Similar to depression, anxiety affects millions of Americans, including veterans, annually. About 9.9% of the veteran population reported feelings of anxiety.8
- Relationship issues: While there is no available data to link relationship issues to increased instances of SUD or to veterans, a strained relationship may contribute to overall stress levels. Unmitigated stress can leave a veteran predisposed to higher instances of substance to cope with those feelings.9
- Sleep deprivation: PTSD is linked to insomnia, which can turn into sleep deprivation. The cycle perpetuates, as symptoms can become exacerbated with lack of sleep, which can further drive someone to substances to cope with their feelings of PTSD and lack of sleep.10
- Combat stress: The stresses of combat may present as PTSD, which can often coincide with substance use disorder. SUD and PTSD commonly co-occur, as presented above.7
There may be other socioeconomic or environmental factors that contribute to a veteran’s use of substances. No 2 veterans are the same, nor should their stories or recoveries be viewed the same.
Veterans and Mental Health Issues
Many veterans return from their service and experience mental health issues. The harsh conditions and traumatic events many see while in active duty can lead to long-lasting mental health conditions. What’s more, other contributing factors, like traumatic brain injuries or other injuries, can alter a veteran’s mental health and negatively affect their quality of life or lead to an increased risk for using substances to cope with their condition.
Traumatic Brain Injury & Veterans
Traumatic brain injury (TBI) is what it is called when someone has a bump, blow, or jolt to the head, or a penetrating head injury that results in disruption to their brain’s function.11 para 1 While TBIs can happen to anyone, service members are at a higher risk for TBI due to the nature of their job.11 para 3
From 2000 to 2019, nearly 414,000 service members had a TBI.11 para 3 Symptoms of TBI can vary greatly but can include behavioral changes, headaches, issues with memory recollection, and sleep impairment.11 para 4 While some mild TBIs may resolve, some may not, and severe TBIs can result in a veteran needing significant assistance in all areas of life.11 para 4 A veteran with a TBI may be at higher risk of using substances to cope with their pain or cognitive impairment.
PTSD & Veterans
Many veterans and active-duty service members experience PTSD. PTSD can occur in anyone but is common with service members since it occurs after someone has experienced something traumatic, and its symptoms often include having unwanted flashbacks of the event, heightened reactions, anxiety, depression, problems sleeping, and night terrors.7 An estimated 500,000 service members in the past 13 years were diagnosed with PTSD.12 “Prevalence of PTSD in Veterans”
Those with PTSD are at a higher risk for developing SUD.7 About 27% of veterans receiving treatment at the VA for PTSD also have SUD.7
Department of Veterans Affairs (VA)
The U.S. Department of Veterans Affairs exists to help connect veterans with the services they need to lead a productive, healthy life.13 Through their VA benefits and healthcare, the VA seeks to help support veterans in all walks of life. Veterans and their families can learn more about substance use, mental health conditions, and the various treatment options available for many of these conditions.13 Reach out to your local VA today to learn how they can help you or your veteran.
Substance Abuse Help for Veterans
If you or a loved one that has returned from combat or service is experiencing substance use disorder or another mental health issue, it’s important to prioritize getting treatment. Pushing treatment down the road can lead to a worsened condition or substance use, which can cause undesirable health conditions.
Getting the appropriate treatment is essential, and it’s beneficial to seek treatment through the VA or other programs that specialize in treating veterans. Attending a veteran-specific SUD treatment program can help ensure that your care is focused on issues unique to veterans.
The VA provides the following treatment options for veterans who are struggling with addiction, SUD, mental health, or all of the above:14 “More information about VA mental health services – What Kinds of Mental Health Services Does VA Provide?”
- Short-term inpatient care for severe or life-threatening mental illness
- Intensive outpatient care
- Standard outpatient care
- Residential (live-in) or rehab programs
- Primary care for common behavioral or mental health problems
- Return-to-work settings
- Emergency mental health care and access to care
- Veterans Crisis Line
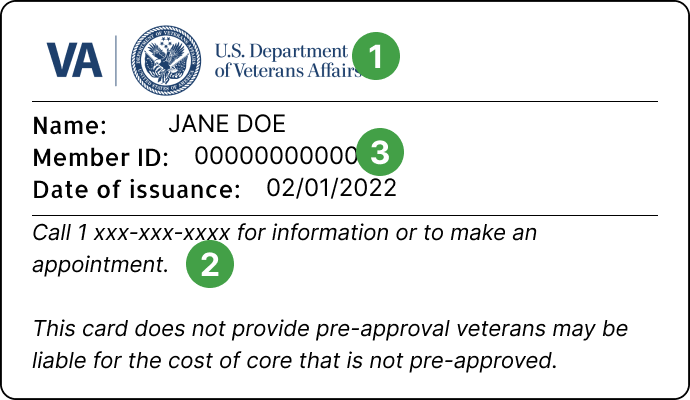
If you have a private health insurance plan, Medicare, Medicaid, or VA health benefits, you may be able to use them to seek care at facilities outside of the VA network. Be sure to look at your insurance card and call the number on the back of your card to find out what may or may not be covered in regards to treatment for your mental health or SUD.
Desert Hope: Salute to Recovery
If you’re looking for a renowned treatment program dedicated to the needs of veterans, the “Salute to Recovery” program offered at Desert Hope Treatment Center in Nevada may be the place for you. The center, which is owned and operated by American Addiction Centers (AAC)—an industry leader in addiction treatment—specializes in helping veterans manage and treat SUD, mental illness, and co-occurring disorders.
AAC works with a wide variety of insurance plans, which means you may be able to use your health plan to cover all or some of the costs associated with treatment at the Salute to Recovery program. To learn more, call the confidential AAC helpline today. You can also enter your insurance information below to verify your benefits and coverage and find out whether this program may be right for you.
Sources
- S. Department of Veterans Affairs. (n.d.). Mental health.
- Inoue, C., Shawler, E., Jordan, C. H., & Jackson, C. A. (2022, May 23). Veteran and military mental health issues.
- National Institute of Drug Abuse. (2019, October). General risk of substance use disorders.
- S. Department of Veterans Affairs. (2022, April). Spotlight on alcohol use disorder (AUD) and substance use disorder (SUD).
- S. Department of Veterans Affairs. (2020, July 30). VA reduces prescription opioid use by 64% during past eight years.
- S. Department of Veterans Affairs. (n.d.). PTSD and substance abuse in veterans.
- National Center for Posttraumatic Stress Disorder. (n.d.). For veterans and families: Understanding PTSD and substance use for veterans, general public, family and friends.
- S. Department of Veterans Affairs. (n.d.). Depression.
- S. Department of Veterans Affairs. (n.d.). Responding better to stress.
- S. Department of Veterans Affairs. (n.d.). Sleep problems in veterans with PTSD.
- S. Department of Veterans Affairs. (n.d.). Traumatic brain injury (TBI).
- Reisman M. (2016, October). PTSD treatment for veterans: What’s working, what’s new, and what’s next.
- S. Department of Veterans Affairs. (2021, September 20). About VA.
- S. Department of Veterans Affairs. (2021, February 12). VA mental health services.