Does UMR Insurance Cover Drug & Alcohol Detox or Rehab Programs?
UMR is a third-party administrator (TPA) for UnitedHealthcare and various employers that offer this option.1 A third-party administrator means they will handle all the processing of claims, pay for services, and manage your insurance benefits package.1 Through your UMR insurance benefits, you can access health care coverage for a variety of issues.
If you are dealing with a drug use disorder, finding appropriate rehab care is vital to your recovery and well-being. With UMR insurance coverage, you can start your journey to sobriety. Search for UMR drug detox treatment nationwide by accessing the provider search tool.
UMR is a preferred provider organization (PPO) insurance plan.2 This type of plan offers several benefits for users, such as:2
- You can see a specialist without a referral.
- You can access a large network of providers, including doctors and hospitals.
- You can receive services at a discounted rate, sometimes up to 30% off.
- You normally don’t have to fill out a lot of forms.
- The facility you want to go to is probably already in the network.
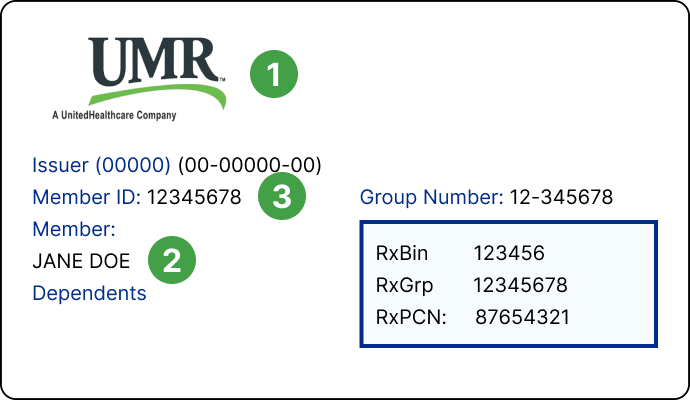
Call the number on the back of your card to contact a UMR administrator who can tell you which drug rehab facilities are within the network and verify your benefits.
Types of Addiction Treatment covered by UMR Health Insurance
Seeking drug rehab requires getting the appropriate treatment plan. You can discuss the particulars of your situation with an admissions navigator to determine what level of treatment is best for you in the beginning. Some people may need to participate in several treatment programs to achieve the best results. For example, you may start at a more intense level of treatment, such as residential care, and taper off to outpatient treatment over time.
You may be wondering about your UMR insurance substance abuse treatment coverage. You don’t have to worry about being denied for a substance abuse issue. According to federal mandates, specifically the Affordable Care Act (ACA), all insurance providers must allow coverage for addiction care, which comes under behavioral health benefits.3 While each plan has specific deductibles and copays, you can count on some type of coverage. The extent of coverage varies depending on the type of policy and tier level you choose.
Some of the UMR drug treatment programs that may be at least partially covered include the following:
- Inpatient residential treatment
- Outpatient rehab treatment
- Psychotherapy
- Intensive outpatient (IOP)
- Partial hospitalization (PHP)
Here is an example of the deductible and copayments for the Premier Plan to give you an idea of associated costs:4
- Substance abuse outpatient services have a $40 copay for an office visit and a 5% coinsurance after a $100 copayment.
- Substance abuse inpatient services have a 5% coinsurance after a $100 copayment.
- Both services have a 50% coinsurance if you use out-of-network providers.
Does UMR Insurance Cover Inpatient Mental Health Treatment facilities?
According to the National Institute on Drug Abuse (NIDA), many people with substance use issues also have mental health disorders.5 About 50% of people who have a substance use disorder get diagnosed with a mental illness at some point.5 It works the other way around, too. Researchers aren’t convinced that substance abuse leads to mental illness or that mental illness leads to substance abuse. In fact, they aren’t always sure which disorder comes first. 5
One thing is for sure, though: you should treat both conditions so that you have a better outcome. Many therapeutic approaches exist alongside detox, so you can treat these in tandem.5 As far as UMR insurance rehabilitation coverage goes, because of the federal mandates mentioned above, you can count on having insurance coverage for both mental health and substance abuse disorders.3
How Long Does UMR Insurance Cover Inpatient Rehab Programs?
The length of UMR drug treatment is between you and your admissions navigator. They will provide a recommendation about what treatment program(s) will be most helpful for your situation and how long it will take. The amount of time your UMR benefits will cover varies depending on what type of policy you have. The NIDA recommends a minimum of 3 months for substance abuse issues.6 You can call the number on the back of your card or look up your plan information to find more information.
What if My UMR Insurance Policy Does Not Cover Inpatient Rehab?
You might be wondering what you should do if your UMR rehab insurance doesn’t cover the particular addiction services you need or doesn’t cover everything. You should still move forward. Putting off your health and wellbeing will only prolong recovery. You do have alternative options; many UMR rehab centers will assist people who don’t have coverage. They may help with financial aid or scholarship options.
Additionally, you can sometimes apply for a sliding scale fee payment plan, which includes a discounted price for services. You might also be able to arrange to pay over time. Consider checking into these options. Whatever happens, don’t delay seeking help for your addiction needs.
UMR Health Insurance In-Network vs. Out of Network Inpatient Rehab Centers
When you have a plan with UMR, you gain access to United Healthcare’s network of providers. They have one of the largest networks in the nation, which means the UMR mental health provider list will be extensive. Finding in-network UMR rehab centers is simple: access the search engine here and put in the location you want to search along with the service you need. If you know the provider’s name, you can type that instead. This will populate results in the area you chose.
How to Check UMR Insurance Coverage for Alcohol and Drug Rehab?
The UMR Health insurance covers drug and alcohol addiction treatment. The PPO plan, through United Healthcare, allows you to work with a provider within the network. For a more seamless experience, American Addiction Centers (AAC) can verify your insurance coverage for you. All you need to do is fill out the form on this page, and you will get an answer immediately. If you’d rather talk to someone in person, contact the AAC helpline by calling and someone will check your benefits right while you’re on the phone.
AAC’s Desert Hope Treatment Center is a highly qualified rehab in Nevada with a wide range of treatments, including co-occurring disorder treatment, medical detox, and more. They are accredited by the Joint Commission for Behavioral Health and also offer special programs for veterans and first responders.
Sources
- (2021). Home.
- (2016). Medical benefits.
- gov. (n.d.). Mental health & substance abuse coverage.
- (2019). Summary of benefits.
- (2018). Comorbidity: Substance Use Disorders and Other Mental Illnesses DrugFacts.
- (2020). Principles of Effective Treatment.