Anthem BlueCross of California For Alcohol And Drug Rehab Programs in CA
Just like all commercial, state-regulated health insurance providers, Anthem California is required by law to provide behavioral health services coverage. This includes substance abuse rehab (alcohol and drug recovery programs) and the necessary treatment for dual diagnosis patients. Anthem Blue Cross California also provides coverage for any related services regarding the overall health of its members.1, 2
Every Anthem California plan offers free preventive care, medication coverage for most frequently used drugs, and predictable out-of-pocket costs. You can also check if you qualify for financial help through the American Rescue Plan. If you do, this can lower your monthly premium.1
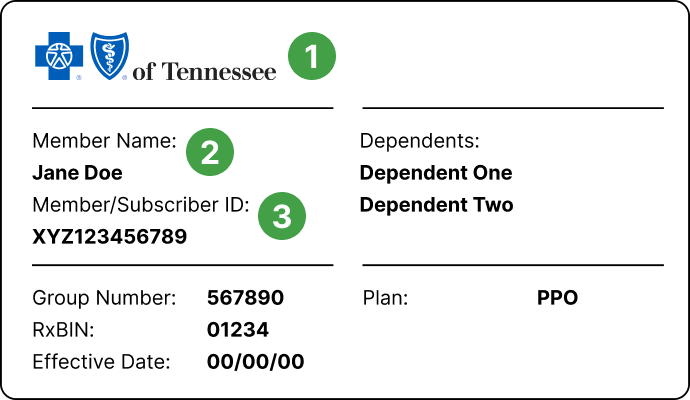
If you already have certain rehabilitation centers in mind, whether because they’ve been recommended to you, or you’ve done your own research, you can call their hotline numbers and provide your insurance information so they can check your coverage and benefits. You can also call the number on the back of your health insurance card and get and get the most accurate information directly from your healthcare provider. Since not all Anthem California healthcare plans offer the same level of coverage, yours will depend on the specific type of plan you have.3

What to Know About Anthem California
Anthem Blue Cross and Blue Shield is one of the largest health insurers in the United States. It serves more than 70 million members through its affiliated companies, which means that one in eight US residents receives health care through Anthem-associated plans. Anthem’s health benefits include behavioral health services, meaning substance abuse and mental health disorders treatment.4
Anthem Blue Cross is the trade name of BC of California, an independent licensee of the Blue Cross Association. Anthem BCBS of California provides coverage and benefits according to current clinical and behavioral health guidelines, as well as federal or state law.5
Under the Affordable Care Act (ACA), every health insurance plan is assigned a ‘metallic’ level. All marketplace plans are divided into 4 “metal” categories based on how you and your plan split the costs of healthcare services you receive. This has nothing to do with the quality of care you receive. The four categories are:6
- Bronze (lowest monthly premium, highest deductible.)
- Silver
- Gold
- Platinum (highest monthly premium, lowest deductible.)
Since 56% of CA rehab facilities accept private insurance, including Anthem of California, finding a suitable substance abuse treatment facility for yourself or a loved one shouldn’t be a challenging task.7
What Kind of Coverage Does Anthem California Insurance Provide for Addiction Treatment?
The elements of each patient’s substance abuse treatment program can vary depending on each person’s individual needs, the severity of addiction, lifestyle, background, belief system, and other factors. However, even though certain approaches and services might be beneficial or even ideal for some patients, they might not comply with the medical necessity criterion.8, 9
Anthem California, like other health insurance providers, covers treatment that is determined to be medically necessary, appropriate, evidence-based, and FDA-approved. The level of coverage will naturally depend on the type of health plan you have (the above-listed categories of Bronze, Silver, Gold, and Platinum plans), and each of them will cover a different percentage of your substance abuse costs.10
As mentioned, medically necessary treatment (determined by a team of substance abuse and mental health specialists) will be covered in all settings:11
- Inpatient/residential rehab is usually recommended for patients who suffer from more severe forms of addiction, as well as those who need to remove themselves from their usual environment and lifestyle to avoid triggers and relapse. This type of treatment program can be short-term or long-term.12, 13
Short-term programs begin with up to a week of medically monitored detoxification and usually last for 28-30 days. More severe forms of addiction warrant long-term rehab programs. They can last for about 3 months, or 90 days if required by the patient’s condition. In most severe cases, frequently those accompanied by co-occurring mental health issues, long-term rehab can even last 6 months, up to a year.12, 13
- Outpatient rehab programs are the most common form of SUD treatment in the U.S. In 2018, 83% of rehab facilities offered outpatient services.14 They are usually recommended to those with less severe forms of addiction, and patients who need flexibility and are unable to take time away from their everyday life responsibilities. These programs generally involve meeting with a counselor/psychotherapist at the rehab center for a few hours, a couple of times every week.12
- Intensive outpatient programs (IOP) involve more hours of treatment and include psychosocial programs. Intensive outpatient treatment is particularly beneficial for people with dual diagnoses, and it is proven that it can increase abstinence. It has also been associated with decreases in psychological symptoms and scores high when it comes to client satisfaction.14
The recommended duration of intensive outpatient programs is usually 90 days. The length of treatment can be modified – increased or decreased depending on each patient’s clinical needs, progress, support system, and other factors. Naturally, longer treatment times are related to better outcomes and longer-lasting sobriety.15 - Partial hospitalization programs (PHP) are best suited for moderate addiction cases and patients who have a stable home environment so there’s no need for them to live at the facility. This type of treatment requires more hours of treatment at the rehab center (starting with 20 hours per week), and it usually lasts for a few months. The intensity of services is higher than in outpatient settings and it includes psychiatric, medical, and lab services in a structured setting.16
Does Anthem Insurance in California Provide Coverage for Mental Health Disorders and & Dual Diagnosis Treatment?
The provisions of the Affordable Care Act (ACA) require that all state-regulated healthcare insurers provide the same level of coverage for behavioral services as they do for other medical conditions, and this includes mental health and substance abuse disorders.17
However, the exact coverage and benefits will depend on each patient’s plan.18 California’s Mental Health Parity Act, amended in 2020, requires commercial health plans to provide full coverage for the treatment of all substance abuse and mental health disorders.2
People suffering from any type of substance abuse disorder often also suffer from a co-occurring mental health disorder. About half of people with a substance use disorder also experience serious mental illness.19
In the state of California, 89.3% of rehab facilities treat patients with dual diagnoses. Almost half (46.5%) of California’s rehab clients were diagnosed with co-occurring mental and substance abuse disorders according to the 2017 National Survey of Substance Abuse Treatment Services (N-SSATS).7
Dual Diagnosis Treatment
It’s often difficult to tell if the mental health issues are the underlying cause of the SUD, or if prolonged use of alcohol or illicit substances caused mental health issues to develop. In either case, one condition can’t be treated successfully without the other. This is why patients entering rehab should be thoroughly assessed for any coexisting condition. Research shows that addressing and treating both disorders simultaneously is the most effective approach for such patients.20
Several types of mental health professionals can collaborate in designing a suitable treatment for such patients and psychiatrists can prescribe appropriate medications if necessary.21
What Length of Alcohol and Drug Inpatient Rehab Programs Do Anthem California Plans Cover?
The length of treatment for substance abuse in an inpatient setting will be covered by Anthem California according to the medical necessity criterion. This means that the treatment must be appropriate, scientifically proven, and FDA-approved if it involves medication. However, since each person’s needs are different it is possible that what’s determined by a team of addiction specialists to be the most effective treatment for a certain patient isn’t always covered by that patient’s plan because of different policies and tiers of coverage.9, 22
Longer treatment times tend to result in longer-lasting recovery and fewer instances of relapse, while a structured inpatient setting helps patients adhere to the program, and their progress is monitored daily. Another benefit of a live-in treatment program is the companionship that forms between patients since they’re going through similar experiences.11, 23
Numerous studies show that group therapy and peer interaction are highly beneficial for recovery. Groups provide social support and reduce feelings of shame and stigma associated with both SUDs and mental health issues. This helps fight the feeling of isolation.24
To be sure what kind of coverage your insurance plan can provide, reach out to your healthcare insurance provider to get accurate information or look up the specifics on your insurance card or in your insurance contract.
What if My Anthem California Policy Doesn’t Cover Inpatient Alcohol or Drug Rehab?
In such cases, you might have to research other payment options for financing your recovery treatment. If you’re not covered through an employer, or eligible for Medicare/Medicaid, you may qualify for federal financial aid. This form of financial help is called a health insurance subsidy, and it was established by the Affordable Care Act (ACA).25
Eligibility for this subsidy depends on your income and household size. Another factor that influences your eligibility is the cost of health coverage in the state you live in.26
Almost half of California’s rehab centers offer free treatment for clients without the financial means to pay for treatment (46.6%), while 61.2% of rehabs offer a sliding fee scale. The option of self-payment is, naturally, available in most CA rehab centers (85.5%).7
Whatever your situation, getting help as soon as possible can prevent more severe substance abuse issues, as well as the development, or aggravation of mental health ones, and even prevent numerous SUD-related health conditions that may develop as a result of prolonged substance use, and the lifestyle that usually follows it.27
Anthem California In-Network vs. Out-of-Network Coverage for Inpatient Drug Rehabs
All Anthem California healthcare plans provide high-quality care through a wide network of primary care physicians, various types of specialists, hospitals, pharmacies, and other related facilities that have contracts with Anthem California. This means that they can provide you with the necessary services at lower rates. Those providers are called in-network providers or preferred providers.28
Healthcare providers who don’t have contracts with Anthem California are out-of-network providers. If you choose to get your healthcare services out-of-network, there’s no guarantee how much you’ll be charged, but it would most likely be a lot more than what in-network providers charge. Additionally, you usually have to file your own claims and pre-approval requests when using out-of-network providers.28
The easiest way to check if a certain provider is in-network with Anthem California is to look it up on their website or call Anthem California helpline and ask a representative.29
How Can I Check My Anthem California Insurance Coverage for Inpatient Drug Rehab Centers?
The easiest and most reliable way is to reach out to Anthem California so you can get accurate information about your healthcare plan coverage. You can look up the details on your insurance card or in your contract. You can also ask your primary care physician for a referral based on their professional evaluation.30
One of the highest-rated in-network substance abuse treatment providers that work with Anthem BlueCross California is the American Addiction Centers (AAC). This is a network of top-notch rehab centers across the U.S. A considerable number of nationwide rehab facilities in-network with all the major insurance providers will make finding an appropriate program near you an easy task.
You can check your insurance coverage and payment options by calling the AAC helpline and speaking to one of the AAC’s admission navigators who can verify your benefits during the call if you have your insurance card with you. You can also fill out a verification of benefits form online and get information about your insurance coverage or alternative payment options.
AAC’s admission navigators can also guide you through the admissions process, explain the intake, evaluation, and the following steps of treatment. They can also help you with the same-day admission if you’re experiencing an acute crisis and wish to start your treatment as soon as possible.
One of the leading local rehab facilities is the Laguna Treatment Center in California. This high-quality rehab center places special focus on medically compromised patients and provides round-the-clock care, using Medication-Assisted Treatment (MAT) if necessary. It offers a full continuum of care so, after medically monitored detoxification process and mitigation of unpleasant withdrawal symptoms, patients move on to evidence-based behavioral therapies, group therapies, and other activities included in their individually tailored treatment programs.
What Approaches & Services for Patients With Particular Needs Are There?
AAC prides itself on individualizing treatment to accommodate each patient’s needs. That’s why, among others, it provides special programs and approaches for:
- Patients in need of continuing care and support during weekends.
- Christian rehab programs for religious clients.
- Gender-specific rehab options for women only.
- Addiction treatment for couples going through recovery together
- Flexible schedule programs for professionals who need to keep up with their work responsibilities.
What Else Should I Know About Addiction and Treatment?
Another way to get accurate information about substance abuse and rehab in general, is to call one of the free and confidential 24-hour addiction hotlines. Trained and understanding California hotline representatives can answer all your questions about addiction treatment and evaluate your situation.This is a good first step if you’re unsure about the severity of your substance abuse or simply not ready to make things official yet. Addiction hotlines are also available to people who want to help their loved ones struggling with addiction. Hotline advisors can assess the situation, explain the signs, symptoms, and dangers of substance abuse and recommend the next steps, or refer you to local rehab centers.31
Sources
1. Anthem. (2022). Insurance Plans For Individuals & Families In California.
2. Department of Managed Healthcare. (2022). Behavioral Health Care.
3. HealthCare.gov. The ‘metal’ categories: Bronze, Silver, Gold & Platinum.
4. Anthem, Inc. (2020). Company History.
5. Anthem. (2022). Information for California.
6. Anthem. (2022). Balancing Health Insurance Costs.
7. Substance Abuse and Mental Health Services Administration. (2018).National Survey of Substance Abuse Treatment Services (N-SSATS): 2017. Data on Substance Abuse Treatment Facilities. Rockville, MD: Substance Abuse and Mental Health Services Administration.
8. BlueShiled California, (2020). Individual and Family plan documents.
9. BlueShield California. (2022). Eligibility and benefits.
10. Anthem. (2022). Understanding Subsidies.
11. Substance Abuse and Mental Health Services Administration. (2015).TIP 45: Detoxification and Substance Abuse Treatment.
12. National Institute on Drug Abuse. (2019). Treatment Approaches for Drug Addiction DrugFacts.
13. FindTreatment.gov. (2019). Treatment options.
14.Substance Abuse and Mental Health Services Administration. (2020).Substance Use Disorder Treatment for People With Co-Occurring Disorders. Treatment Improvement Protocol (TIP) Series, No. 42. Rockville, MD: Substance Abuse and Mental Health Services Administration.
15. Center for Substance Abuse Treatment. 2006. Chapter 3. Intensive Outpatient Treatment and the Continuum of Care. Substance Abuse: Clinical Issues in Intensive Outpatient Treatment. Rockville (MD): Substance Abuse and Mental Health Services Administration.
16. Medicaid Innovation Accelerator Program. (2017). Overview of Substance Use Disorder (SUD) Care Clinical Guidelines: A Resource for States Developing SUD Delivery System Reforms.
17. HealthCare.gov. Affordable Care Act (ACA).
18. Blue Shield of California. (2022). Plans.
19. FindTreatment.gov. (2019). Understanding mental health.
20. National Institute on Drug Abuse. (2020). How do other mental disorders coexisting with drug addiction affect drug addiction treatment?.
21. Anthem. (2020). Finding the Right Mental Healthcare for You.
22. National Institute on Drug Abuse. (2012).Principles of Drug Addiction Treatment: A Research-Based Guide, Third Edition.
23. National Institute on Drug Abuse. (2021). Treatment for Alcohol Problems: Finding and Getting Help.
24. American Psychological Association. (2017). Power in Numbers.
25. HealthCare.gov. Subsidized Coverage.
26. HealthCare.gov. Income levels & savings.
27. Ettner, S. L., Huang, D., Evans, E., Ash, D. R., Hardy, M., Jourabchi, M., & Hser, Y. I. (2006). Benefit-cost in the California treatment outcome project: does substance abuse treatment “pay for itself”?. Health services research, 41(1), 192–213.
28. Anthem. (2021). Understanding Your Health Plan’s Network.
29. Anthem. (2022). Find care.
30. Anthem. (2020). Finding the Right Mental Healthcare for You.
31. Zeavin, Hannah. (2020).The Third Choice: Suicide Hotlines, Psychiatry, and the Police.
32. Anthem Blue Cross California. (2021). Covered and Non-Covered Services (Medi-Cal).
33. BlueShield California. (2022). Medication policy user guide.
34. BlueCross BlueShield. (2022). Nationwide access and local support: What it means for Blue members.