Cigna Insurance Coverage for Drug and Alcohol Rehab Treatment
Deciding to seek treatment for drug addiction can be very challenging. One reason is the cost associated with drug addiction treatment. Using health insurance can make addiction treatment more affordable.
The goal of this guide is to make the decision to seek drug addiction treatment for you or your loved one easier by offering detailed information about the drug treatment coverages provided by Cigna Insurance.
What is Cigna Insurance?
Cigna is a worldwide health service company that serves more than 178 million people around the globe, provided medical healthcare coverage for 15 million customers in the U.S.1
In addition to providing coverage for medical and surgical services, Most Cigna plans are required by law to provide health insurance coverage for the treatment of behavioral health issues like addiction and other mental illnesses such as anxiety and depression.2
What Are The Different Cigna Health Insurance Plan Types?
Cigna offers individual and family plans that may be purchased on the Healthcare Marketplace or group insurance plans offered through employers.
Cigna individual and family insurance plans include:3
- Cigna HMO requires you to use only the doctors and hospitals within a specified network. An HMO often has lower monthly premiums, but higher deductibles. Under an HMO, you will choose a primary care physician who will assist with coordinating your care.
- Cigna EPO offers a specific network of doctors and hospitals you must use. While the premiums for an EPO may be lower than an HMO, the deductibles may be higher, and services received from doctors and hospitals outside of the network will not be covered unless it is an emergency.
- Cigna PPO offers a large network of doctors and hospitals you are required to use. The policy premiums of a PPO are typically higher than an HMO, but your deductibles may be lower or higher.
Cigna plans that may be offered by employers include:
- Cigna Open Access Plus (OAP) offers a national network of doctors and hospitals, discounts, the option to select a primary care provider (PCP), and no referral requirements.4
- Cigna LocalPlus® provides employees with a limited network of doctors and hospitals plus access to Away from Home Care.5
- Cigna SureFit® is a customizable plan for employers and employees and is available only in certain service areas.6
- Cigna Indemnity Plans (Network Savings Program) allow employees to see any doctor, use any hospital, and visit any specialist without a referral.7
- Cigna Group Medicare plans are designed to meet the specific needs of retired employees.8
There are several drug rehabs in the Cigna network. A rehab facility can help you check your insurance coverage. For example, American Addiction Centers (AAC), which accepts Cigna, has a webpage where you can enter your policy number to instantly verify your drug rehab coverage.
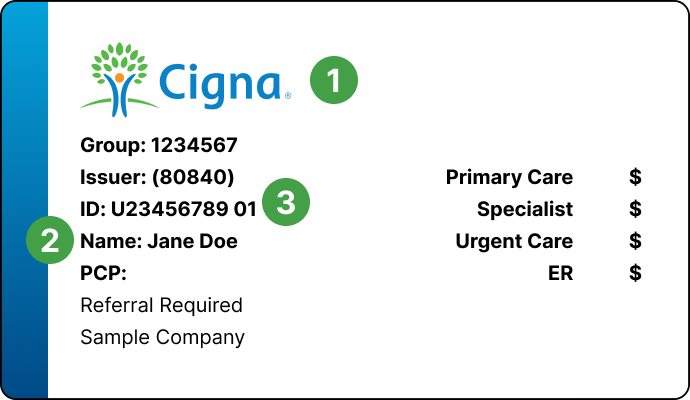
You can also call the telephone number listed on the back of your Cigna insurance card to verify coverage.
Does Cigna Insurance Cover Rehab for Drugs and Alcohol?
Yes. Cigna insurance plans will likely cover addiction treatment. Due to the passage of the Affordable Care Act (ACA), insurers like Cigna are required to provide coverage for addiction treatment.2
The extent of this coverage however, will vary based on the individual insurance policy.
What Treatment Programs Does Cigna Cover?
Drug treatment coverages differ across Cigna’s plans. Your plan may cover the following services for the treatment of alcohol, heroin, prescription opioid, marijuana, methamphetamine, cocaine, benzodiazepine, prescription stimulant, and sedative addiction:9
- Medical detox. Detox is utilized to stabilize patients through acute withdrawal under medical supervision. While a necessary step for many patients suffering from addiction, most need continued treatment after detox to remain in recovery.
- Inpatient/residential rehab. Inpatient/residential rehab may require you to stay at a rehab center for 30-120 days, depending on your needs. After the inpatient portion of treatment is complete, you will likely be required to have outpatient rehab and therapy as part of your aftercare plan. Outpatient rehab and therapy may continue for months.
- Outpatient rehab/therapy. Outpatient rehab therapy often involves several weekly therapy and peer support sessions and, if needed, the administration of medications for substance use disorder. There are several levels of outpatient care, including partial hospitalization programs (PHPs) that require 5-7 days a week spent in treatment, intensive outpatient programs (IOPs), which require a minimum of 3 days a week in treatment, and standard outpatient care that affords more flexibility.10
The length of drug rehab treatment varies from person to person based on their needs.
Most plans will require patients to reach a deductible (a fixed yearly dollar amount paid out-of-pocket for healthcare services before Cigna begins covering treatment.11 Other out-of-pocket costs may include copayments or a co-insurance percentage. A copayment is a fixed dollar amount paid by the patient at the point of service (e.g., to see a doctor).12 Co-insurance rates are a percentage of the total cost of a service paid by the patient while Cigna covers the remainder.13
The amount you pay will depend on the type of Cigna Insurance plan you have. To check your Cigna Insurance drug treatment coverage, call to speak with an AAC admissions navigator.
Does Cigna Insurance Cover Mental Health Treatment?
The ACA requires most insurance policies to provide coverage for mental health care and treatment.2 Some people have co-occurring disorders—drug addiction and mental health disorders—requiring simultaneous treatment for both. Effective drug rehab programs are equipped to assist people with co-occurring disorders.9
To check your specific drug treatment coverage under Cigna, speak with an AAC admissions navigator at .
How Long Does Cigna Insurance Cover Rehab?
The duration of drug and alcohol rehab services covered by Cigna Insurance will depend on the type of plan you have. There are several ways to determine what your plan will cover:
- Call the member information number on the back of your card.
- Call AAC at and speak with an admissions navigator.
- Check the Summary of Benefits and Coverage (SBC) documentation for your Cigna plan.
What if My Cigna Insurance Policy Does Not Cover Drug Rehab?
If your Cigna Insurance plan does not cover drug rehab services, know that some drug rehab centers, including AAC facilities, offer payment plans. Call to discuss payment plans at AAC.
Some facilities charge on a sliding scale based on someone’s income and nonprofit organizations may also offer scholarships for both inpatient and outpatient drug rehab services.
Cigna Insurance In-network Vs. Out-of-network Rehab Centers
Cigna Insurance maintains an extensive list of in-network doctors, hospitals, and facilities. In-network refers to a professional relationship that exists between Cigna and the doctor, hospital, and facility. While some Cigna Insurance plans allow for out-of-network care, there may be additional out-of-pocket expenses.14
How To Check Cigna Insurance Rehab Coverage?
Navigating through the many parts of drug treatment coverage under Cigna can be difficult. AAC can help you with this process. You have a few options to get this assistance:
- Fill out the insurance verification form by entering your insurance carrier (Cigna) and policy membership identification number (located on the front of your Cigna Insurance card)
- Call the AAC at and speak with an admissions navigator.
Frequently Asked Questions
Sources
- Cigna. Facts about Cigna.
- U.S. Department of Health and Human Services. (2023, April 20). Does the Affordable Care Act cover individuals with mental health problems?
- Cigna.(2021). What’s the difference between an HMO, EPO, and PPO?
- Cigna. (n.d.). Open Access Plus (OAP) Plans.
- Cigna. (n.d.). LocalPlus Plans.
- Cigna. (n.d.). Cigna SureFit Plans.
- Cigna. (n.d.). Medical Indemnity Plan.
- Cigna. (n.d.). Cigna Healthcare Group Medicare Plans.
- National Institute on Drug Abuse (2018, January). Principles of Drug Addiction Treatment: A Research-Based Guide (Third Edition).
- Center for Substance Abuse Treatment. (2006). Substance abuse: clinical issues in intensive outpatient treatment. Treatment improvement protocol (TIP) series 47. DHHS publication no. (SMA) 06-4182. Rockville, MD: Substance Abuse and Mental Health Services Administration.
- HealthCare.gov. (n.d.). Deductible.
- HealthCare.gov. (n.d.). Copayment.
- HealthCare.gov. (n.d.). Coinsurance.
- Cigna. (2022). In-Network vs. Out-of-Network Providers.
- Centers for Medicare & Medicaid Services. (n.d.). The Mental Health Parity and Addiction Equity Act (MHPAEA).
- Cigna. (2020). Cigna Standards and Guidelines/Medical Necessity Criteria.